Table of contents
Male infertility affects a staggering number of couples worldwide. While the causes range from genetic disorders to lifestyle choices, understanding the root of the problem is pivotal. This article delves into the intricate world of male reproductive health, shedding light on the leading causes of infertility in men and offering a beacon of hope through potential treatments and preventative measures.
Risk Factors and Causes of Male Infertility
The World Health Organization defines infertility as the inability to achieve pregnancy after one year of unprotected intercourse. 1 out of 6 Canadian couples experience infertility. 3 out of 10 times, men are the cause of infertility. While certain cases of male infertility are due to anatomical abnormalities and ejaculatory disordfers, a large fraction of cases are due to deficient or abnormal production of sperm. Fortunately, many cases of male infertility are reversible and can be corrected.

Types of Male Infertility
To navigate the complex domain of male reproductive health, it's pivotal to distinguish between temporary and permanent male infertility causes. Shedding light on these categories provides invaluable understanding for individuals exploring fertility concerns.
Temporary Male Infertility:
- Infections: Conditions such as mumps orchitis can temporarily impair sperm quality and count.
- Ejaculatory Dysfunction: Certain situational factors might lead to ephemeral ejaculatory challenges.
- Lifestyle and Environmental Factors: Key factors include:
- Alcohol and Male Fertility: Excessive alcohol intake can momentarily reduce sperm quality and count.
- Drug Use: Recreational drugs have been known to cause brief fertility disruptions.
- Stress: Chronic or severe stress can interfere with hormones crucial for sperm production.
- Heat Exposure: Regular visits to saunas or hot tubs can diminish sperm count for a short duration.
- Medication Effects: Some medications influence sperm production, but fertility typically rebounds upon cessation.
- Retrograde Ejaculation: This issue can occasionally be induced by certain drugs, resulting in semen flowing back into the bladder.
Permanent Male Infertility:
Testicular Causes:
- Varicocele: If untreated, this condition might lead to enduring infertility challenges.
- Trauma: Significant or recurrent testicular injury can have irreversible effects.
- Congenital Anomalies and Undescended Testes: The latter, if not rectified in early stages, becomes a permanent infertility factor.
- Genetic Disorders: Syndromes like Klinefelter impact sperm genesis.
Post-testicular Causes:
- Vas Deferens Absence: Typically observed in ailments like Cystic Fibrosis.
- Ductal Blockages: Permanent blockages impede the sperm's journey, preventing its release.
Sperm-specific Concerns:
- Azoospermia: In certain cases, the complete absence of sperm production, especially from genetic origins, is permanent.
- Immunological Issues: Despite treatment, consistent anti-sperm antibody production by the immune system can perpetuate infertility.
- Environmental Toxins and Infertility: Prolonged exposure to harmful toxins, radiation, or chemicals can irreversibly damage male fertility.
Prevention and Treatment Options for Male Infertility
There are so many other risk factors that contribute to the development of infertility that has not been mentioned in this article. Examples include alcohol-derived liver damage (cirrhosis), fatty liver disease, psychological stress, and some sexually transmitted infections such as chlamydia In this article, we are going to outline some behavioral and lifestyle modifications that can foster reproductive health benefit.
Scrotal Heat: How it Affects Male Fertility and Remedies
Exposure to heat has a deleterious effect and is considered a significant risk factor for male infertility. Increased scrotal temperature can lead to hormonal imbalances that increase sperm cell death. For example, varicocele, a disorder characterized by the loss of the ability to regulate the temperature of the testes, is the most common cause of infertility and affects about 15% of the male population.
Some risk factors for accumulation of heat (hyperthermia) in the scrotum include prolonged sedentary time (lack of air circulation and increased heat transfer from thighs), obesity, occupational heat exposure (in the case of baking or welding), high environmental temperature and seasonality (higher incidence in summer compared to winter), and using a laptop in a lap position close to genitals. Accordingly, scrotal cooling can improve sperm count, motility and function.
Physical Activity's Role in Boosting Male Fertility
Light physical activity increases movement of legs that allows for better ventilation and dissipation of heat. Simple but significant measures can be taken to reduce the impact of heat stress. This includes preventing sitting for an extended amount of time, wearing clothing that does not restrict genital airflow, maintaining a healthy weight, and modifying behavior such as avoiding sauna and hot baths.
Exercise is an effective way of enhancing reproductive health. Resistance and moderate-intensity aerobic exercise improve fertility by promoting testosterone production. In contrast, long term exhaustive aerobic exercise can worsen sperm quality and harm the reproductive potential
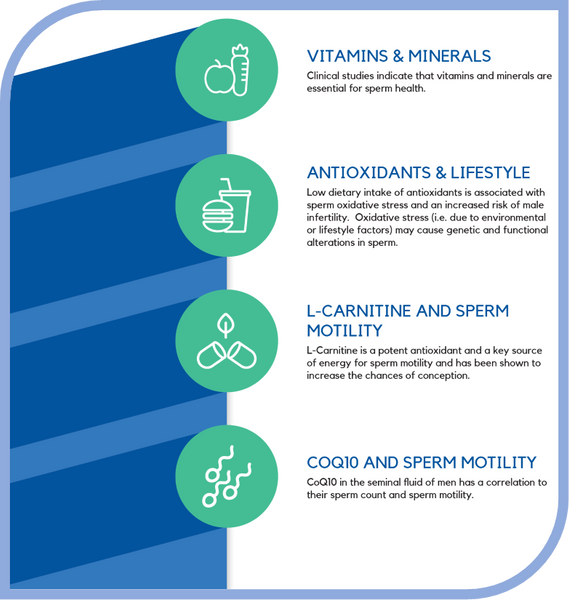
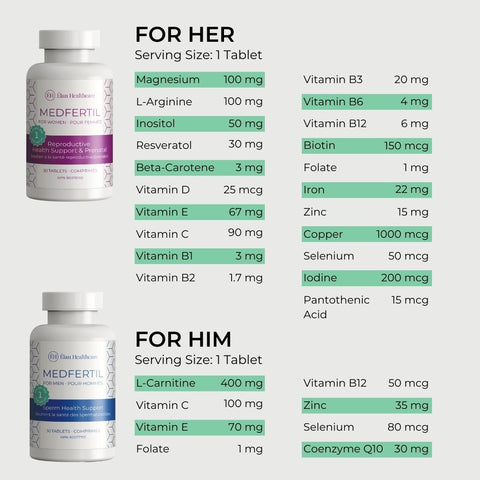
Dietary Supplements and Nutrients: Enhancing Male Fertility
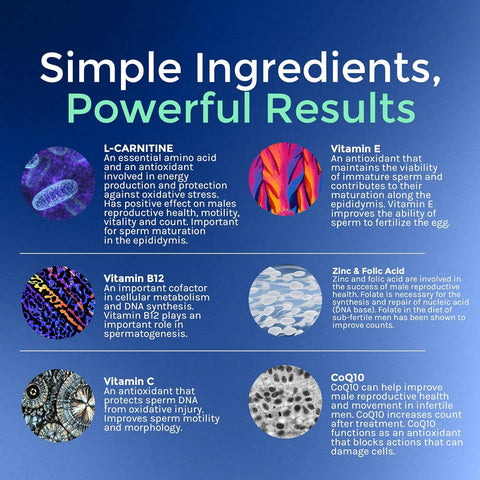
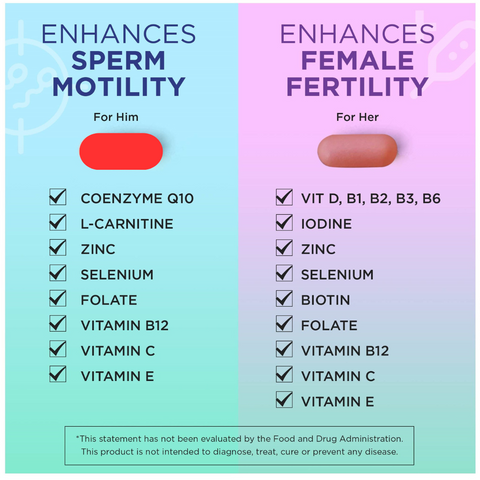
Research suggest that supplementary intake of certain factors can enhance reproductive health. For example, carnitine provides the body with an energetic substrate that enhances sperm motility and maturation.
Zinc deficiency is associated with decreased testosterone levels and sperm count. Subsequently, an adequate amount of zinc intake ensures proper sperm motility and production. Studies have shown that low levels of vitamin C lead to infertility and increased damage to sperm’s genetic material.
Vitamin E is a well-documented anti-oxidant and has shown to prevent infertility. Oral vitamin E supplementation improves sperm quality, resulting in higher probability of achieving pregnancy. Glutathione and selenium are vital to the sperm antioxidant defense.
Deficiency of these supplements leads to defects in sperm motility. Lastly, coenzyme Q-10 is used for energy production in sperm and it also has an anti-oxidant function The take-home message is that an anti-oxidant rich diet concurrent with a suitable supplementation regimen is an effective way in enhancing reproductive health.
Author: Parsa Nafari, Bachelor of Science, Kinesiology
Reviewed by: Dr. Pari Saharkhiz, M.D.
References:
- Canada, P. (2020). Fertility - Canada.ca. Retrieved 1 Feb 2020, from https://www.canada.ca/en/public-health/services/fertility/fertility.html
- Guthauser, B., Boitrelle, F., Plat, A., Thiercelin, N., & Vialard, F. (2013). Chronic excessive alcohol consumption and male fertility: a case report on reversible azoospermia and a literature review. Alcohol and Alcoholism, 49(1), 42–44. https://doi.org/10.1093/alcalc/agt133
- Karmon, A. E., Toth, T. L., Chiu, Y.-H., Gaskins, A. J., Tanrikut, C., Wright, D. L., Hauser, R., & Chavarro, J. E. (2017). Male caffeine and alcohol intake in relation to semen parameters and in vitro fertilization outcomes among fertility patients. Andrology, 5(2), 354–361. https://doi.org/10.1111/andr.12310
- Qiao, Z.-D., Dai, J.-B., & Wang, Z.-X. (2015). The hazardous effects of tobacco smoking on male fertility. Asian Journal of Andrology, 17(6), 954. https://doi.org/10.4103/1008-682x.150847
- Jurewicz, J., Dziewirska, E., Radwan, M. ł., & Hanke, W. (2018). Air pollution from natural and anthropic sources and male fertility. Reproductive Biology and Endocrinology, 16(1). https://doi.org/10.1186/s12958-018-0430-2
- 6 Air Quality Health Index (AQHI). (2020). Ontario. http://www.airqualityontario.com/aqhi/
- Yan, J.-G., Agresti, M., Bruce, T., Yan, Y. H., Granlund, A., & Matloub, H. S. (2007). Effects of cellular phone emissions on sperm motility in rats. Fertility and Sterility, 88(4), 957–964. https://doi.org/10.1016/j.fertnstert.2006.12.022
- Noorimotlagh, Z., Haghighi, N. J., Ahmadimoghadam, M., & Rahim, F. (2016). An updated systematic review on the possible effect of nonylphenol on male fertility. Environmental Science and Pollution Research, 24(4), 3298–3314. https://doi.org/10.1007/s11356-016-7960-y
- urewicz, J., Radwan, M. ł., Wielgomas, B., Kałużny, P. ł., Klimowska, A., Radwan, P. ł., & Hanke, W. (2017). Environmental levels of triclosan and male fertility. Environmental Science and Pollution Research, 25(6), 5484–5490. https://doi.org/10.1007/s11356-017-0866-5
- Maske, P., Dighe, V., Mote, C., & Vanage, G. (2020). n-Butylparaben exposure through gestation and lactation impairs spermatogenesis and steroidogenesis causing reduced fertility in the F1 generation male rats. Environmental Pollution, 256, 112957. https://doi.org/10.1016/j.envpol.2019.112957
- Banihani, S. A. (2019). Effect of aspirin on semen quality: A review. Andrologia, 52(1). https://doi.org/10.1111/and.13487
- Sinclair, S. (2000). Male infertility: nutritional and environmental considerations. Altern Med Rev, 5(1):28-38.
- Plessis, S. D. S., Agarwal, A., & Jr., E. S. S. (2016). Testicular heat stress and sperm quality. In Male infertility: a complete guide to lifestyle and environmental factors (Softcover reprint of the original 1st ed. 2014 ed., pp. 105–125. Springer.
- Plessis, S. D. S., Agarwal, A., & Jr., E. S. S. (2016). The impact of physical exercise on male fertility. In Male infertility: a complete guide to lifestyle and environmental factors (Softcover reprint of the original 1st ed. 2014 ed., pp. 47-60. Springer.
- Begum, H., Moniruddin, A. B. M., & Nahar, K. (1970). Environmental and Nutritional Aspect in Male Infertility. Journal of Medicine, 10(1), 16–19. https://doi.org/10.3329/jom.v10i1.1997

























No comments yet.
There are no comments for this article. Be the first one to leave a message!
+ Open to leave a Comment